Knee Arthritis
What is it?
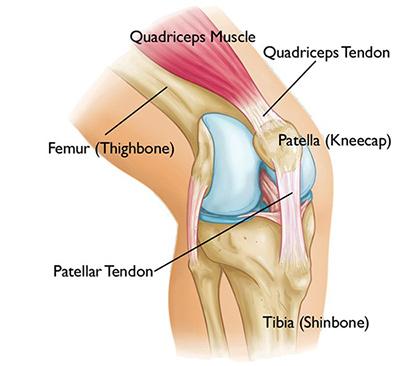
The ends of the thigh bones and the tops of the leg bones with the knee cap make up the knee joint. Arthritis means inflammation of the joint. There are several types of “arthritis”. In the knee the most common is the “wear and tear” arthritis called osteoarthritis. Symptoms of osteoarthritis often include swelling, pain with activities, and “grinding or popping”. Inside the knee the ends of the bones are covered with a smooth coating called articular cartilage (blue surfaces in the picture below). The surfaces are very smooth and a small amount of fluid, called synovial fluid, lubricates the knee. In osteoarthritis the smooth coating can crack, peel off, and eventually lead to exposed bone. Often people feel the knee can crack, pop, or grind. When the worn-down surfaces are rough, the joint often will swell and be filled with fluid. Some people have referred to this as “water” in the knee.
Knee Arthritis
Treatments Options
Non-Surgical options
Exercises/ physical therapy: Certain exercises for the knee, hip, and gait can help strengthening the knee. Exercises can improve function and pain even with osteoarthritis. Exercises done with the supervision of a therapist may be helpful.
Weight management: For every pound of weight loss, there will be 2-5 times less joint contact pressure in the knee with daily activities.
Medications: non-steroidal anti-inflammatory medications (NSAIDs) such as ibuprofen (advil/motrin), naproxen (aleve), or prescription medications can manage knee swelling and pain. Opiates or narcotics for knee osteoarthritis pain is rarely indicated.
Injections
Corticosteroid injections (a.k.a. steroid injections): This is a strong anti-inflammatory medication that is injected into the knee joint to help with swelling and pain. This injection may be painful at the injection site or in the joint for a few days after the injection. Steroid injections usually provide a few months of relief. However, multiple injections may cause side effects. It is usually given 3-4 months apart. Steroid injections can cause a spike in the blood sugars and those with diabetes are more susceptible.
Visco-supplementation injections (a.k.a. hyaluronic acid or lubrication shot, rooster comb injection): This type of injection involves injecting high concentrations of a protein called hyaluronic acid, which is found in joint fluid or synovial fluid. The synovial fluid in the joint lubricates the knee and significantly lowers the friction at the surfaces. Hyaluronic acid was first purified from a rooster’s comb, but today, most are made synthetically. This type of injection is usually given in a series of 3 to 5 injections, one week apart. Hyaluronic acid can improve the pain and swelling for about 6 months in some patients. The most common side effect is pain at the injection site. Prior insurance authorization may be required.
Biological injections (a.k.a. Platelet Rich Plasma “PRP injections”): In orthopedic surgery biological injections, such as platelet rich plasma (PRP injections) or bone marrow aspirates, have gained interest in the community recently. There are almost 30 studies that reported benefits of injecting plasma from your own blood into arthritic knees. PRP has been used to treat soft tissue injuries such as tendinitis of the elbow, knee, and achilles. The process involves an in-office blood draw from the arm. The blood is then spun down with a machine to separate the platelets. The platelet portion of the plasma contains many proteins that are important in repairing tissue. The patient’s own platelets are then injected into the joint or tendon. Recent research studies have favored PRP injections over hyaluronic acid injections in patients with knee arthritis. One study published in the American Journal of Sport Medicine gathered a group of patients with knee arthritis and randomized them to receive either a PRP injection or an injection with saline. Those with the PRP injection reported 40-50% improvement in function and their pain was reduced in half at 6 months. Another study, published in the Clinical Journal of Sport Medicine from the Hospital of Special Surgery, found the articular cartilage volume was preserved at 1 year after PRP injection. Most research indicate more clinical improvements in patients with mild to moderate arthritis. There is evidence that those with moderate to severe arthritis may benefit as well.
Bone marrow aspirates are another option to obtain cells with the potential of regenerating living tissue. This process involves harvesting cells in bone marrow that is stored in your pelvic bones. Certain cells have the ability to repair damaged tissues and have been used in many fields of medicine including orthopedics, cardiovascular, and autoimmune disorders. In orthopedic surgery, bone marrow aspirates have been shown to heal fractures. There is on going research that isolates specific cells in the bone marrow and shows its potential to regenerate damaged tissues in joints.
Surgical options
Arthroscopy: Using a high-powered camera, the orthopedic surgeon can look inside the knee with very small incisions. The surgeon may be able remove swollen tissue or a torn meniscus with special instruments. Mild arthritis (cracks or frayed cartilage) sometimes can be shaved arthroscopically. This usually involves trimming the rough edges of the cartilage until it is smoother. However, the damaged cartilage and the worn-down surfaces may continue to progress with time. Pain relief, therefore, may be short lived.
Knee Replacement: The worn-out parts of the knee can be replaced with metal and a dense plastic bearing. The can be a “total knee replacement” which includes the knee cap or a partial knee replacement. A partial knee replacement is usually done for those patients with a single worn out area of the knee.
Alternatives to knee replacement: In the young active population, many people may not be ready for a knee replacement or are unwilling to accept the limitations of a knee replacement. Biological options with PRP can be an alternative. Nearly 30 scientific studies have been done with PRP injections and have been shown to be favorable compared to the alternative. Recently a new option, is taking cells from the hip bone marrow and inject them into an arthritic joint. These cells may have the potential to replenish worn out cartilage in some patients.
Alternative surgeries: arthroscopy with microfracture is the drilling of holes in the knee to bring blood and cells with the potential to heal or fill a defined area of worn out cartilage. Long term studies in selected younger patients have been shown to be beneficial for several years. Another option is osteochondral autograft/allograft transplantation (OATs). This involves taking normal cartilage with a bone plug and transferring it to the area in the knee that has worn out. This technique has improved pain and function in the young and active populations. Cartiform and Bio cartilage are similar to OATS but it involves transferring cartilage with no bone, from a donor tissue, to replace the worn out area in the knee and often used in larger defects. High tibial osteotomy is usually done in the younger patient with arthritis limited to one side of the knee and they are not qualified for a partial knee replacement. This is done by cutting the tibia (shin bone) to realign the knee joint, which decreases the contact on the affected side of the knee.

